Researchers affiliated with Driv and their research
Researchers affiliated with Driv study a variety of topics within translational research. Here, you can get to know the different areas and find information about research projects, research groups, and other initiatives related to the field.
Early embryonic BRCA1 epimutations and female cancer
Contact person: Stian Knappskog
In early embryonic life, before any influence of the embryo’s own hormones, the differences between females and males are few. A major difference, however, is that female embryos have two active X-chromosomes during the first 4-5 days while males have one, and that the females thereafter undergo X-chromosome inactivation to secure that only one allele is active per cell. We believe that aberrant epigenetic events (epimutations) occurring before and/or during X-chromosome inactivation is an underlying cause of a large fraction of female cancers and potentially also many other female diseases.
Triple-negative breast cancer (TNBC) is the most aggressive form of breast cancer. Around 5% of cases are caused by inherited pathogenic genetic variants in the BRCA1 gene, while the vast majority remain unexplained and are considered “sporadic”. We recently made a major breakthrough, discovering that normal cells with BRCA1 epimutations are present in a low-level mosaic pattern, in 5-10% of healthy females, and that this significantly increases the risk of TNBC. Our data indicate that a staggering 20% of TNBC cases may be caused by underlying BRCA1 epimutations. Since this mosaicism affects tissues of all germ layers and is present in newborns, the epimutations must occur early during embryonic development.
The timepoint and mechanism for BRCA1 epimutations occurrence, as well as the distribution of such epimutations in the cancer prone tissues, remain unknown. To address this, we will deliver three main outputs: (i) we will identify the precise timepoint of BRCA1 epimutation occurrence, by assessing epimutation concordance in monozygotic twins with known time of split, and by single cell lineage tracing; (ii) we will determine the impact of X-chromosome dosage; (iii) we will map the spatial distribution of BRCA1-epimutated cells in normal breast tissue to reveal if they are clustered in some high-risk milk ducts or regions of the breast.
The project will open new research horizons, far beyond BRCA1 and breast cancer, as our findings will shed light on mechanisms highly relevant for other tumor suppressor genes and female cancers. The results can also be generalized as a concept beyond the field of oncology, as early embryonic epimutations may be a major undiscovered cause of many female diseases other than cancer.
Research on ovarian cancer
Contact person: Line Bjørge
Ovarian cancer affects around 500 women in Norway annually, and despite initial treatment response, most experience relapse. Our research takes a comprehensive approach to the disease, aiming to develop more precise and effective treatment strategies. Through the project portfolio Rethinking Ovarian Cancer (RETHINK), we combine advanced tumor profiling, preclinical models, antibody-based therapies, and clinical translation. We are developing 3D tissue models, multi-omics tools for deep tumor profiling, and innovative immunotherapeutic solutions, including surgery-assisted immunotherapy.
Our research team, known as INOvA (Innovative Novel Ovarian Cancer Treatment Approaches), has existed for over 15 years and is based on interdisciplinary collaboration between researchers and clinicians, supported by national and international research funding. We actively work to understand the tumor microenvironment and identify new biomarkers and treatment options that can improve precision medicine for patients with ovarian cancer.

Early Menopause and Autoimmunity
Contact person: Eystein Husebye
The Center for Premature Menopause and Autoimmunity is a four-year research project funded by the University of Bergen, Helse Bergen, and the Trond Mohn Foundation, led by Professor Eystein Husebye.
The center researches premature ovarian insufficiency (POI), a condition where the ovaries cease to function normally before a woman reaches the age of 40, affecting approximately 3% of women. This results in early menopause and hormonal disturbances. In addition to infertility, the consequences of POI include an increased risk of cardiovascular disease, osteoporosis, dementia, and autoimmune diseases. Hormone treatment can counteract menopausal symptoms associated with POI, but there is currently no treatment to restore or improve fertility. Despite these serious health consequences for women, the cause of POI remains unknown in the majority of cases, and the disease mechanisms are understudied.
POI is a heterogeneous disorder with many different causes, where autoimmunity accounts for 3-30% of cases. In these women, the underlying cause is an immune attack on the ovaries, leading to functional damage. The gradual destruction of the ovaries provides a potential window to halt the immune attack through immunotherapy. Establishing a clear autoimmune cause for POI is therefore important but remains challenging, as ovary-specific autoantibodies have yet to be identified, highlighting the need for better diagnostic tests.
Furthermore, the mechanisms by which sex hormones modulate the immune system and influence the risk of autoimmunity are still unclear, although we and others have previously shown a high prevalence of autoimmune disease in women with POI. Exploring changes in the immune system of young women in menopause could clarify estrogen's role in the development of autoimmune diseases.
Through interdisciplinary national and international collaboration, this project aims to provide unique insights into a disease with devastating consequences for young women, uncover sex-specific features of the immune system, and bring diagnostic tools and new immunomodulatory treatments to the clinic with the goal of restoring fertility.
The project's main goal is to improve diagnostic accuracy and treatment of ovarian failure.
This will be achieved through four work packages:
(1) Identify new autoantigens and autoantibodies targeting ovarian cells in women with POI - led by André Sulen
Identifying autoantibodies that are entirely specific to the disease will enable rapid and accurate diagnosis of whether patients have an autoimmune cause behind ovarian failure and facilitate appropriate treatment. We will use a method called PhiP-seq, in collaboration with Mark Anderson (UCSF, USA), to identify potential autoantibody candidates in serum from women with POI. Findings will be verified in a laboratory setting. We will also compare results with serum from men with autoimmune diseases to ensure the antibodies are specific to women. If promising autoantibodies are found, they will be further developed to determine if they can be used for clinical diagnostics.
Once autoantibodies are identified, we will examine how their targets (antigens) are expressed in cells, including in which tissues, quantities, and in relation to local immune cells. This will enhance our understanding of how the disease progresses. We will also use other organs and publicly available datasets to determine whether this is specific to ovarian cells.
(2) Identify how estrogen deficiency contributes to pathogenic pathways in autoimmune diseases - led by Bergithe Eikeland Oftedal
To identify estrogen's influence on the immune system and how it contributes to autoimmune diseases, we will use single-cell RNA sequencing, combined with in vitro studies of primary immune cells and flow cytometry analysis of blood cells from POI patients. These exploratory studies will provide insights into estrogen's role in the development of POI and generate new hypotheses about disease mechanisms. This information is crucial for developing new treatment strategies and will inform potential immunomodulation strategies to reverse POI. The broad screening of cytokines may also identify useful biomarkers for autoimmune POI.
(3) Determine the genetic contribution to POI - led by Eirik Bratland and Elinor Vogt
We will use exome sequencing to identify the genetic contribution to POI. Exome sequencing allows for the analysis of all coding regions of the genome. By sequencing the exomes of women with autoimmune POI, researchers can identify genetic variants that may contribute to the development of the condition. This includes both known and new mutations in genes involved in ovarian function and autoimmunity. Identifying such variants can provide insights into the molecular mechanisms behind POI and potentially reveal new therapeutic targets.
After identifying genetic variants through exome sequencing, it is important to conduct functional studies to understand their biological significance. This involves investigating how the identified variants affect gene and protein function. For example, researchers may use cell culture models to study the effect of mutations on cell growth, differentiation, and survival. Functional validation is crucial to confirm that the identified variants actually contribute to POI and are not just random findings.
(4) Immunotherapy for autoimmune oophoritis - led by Marianne Øksnes and Elinor Vogt
In a previous smaller study in collaboration with the Karolinska Institute, we showed promising results for improving fertility in women with autoimmune POI using immunomodulatory therapy. We will now expand this study into a multicenter, double-blind, placebo-controlled, randomized trial investigating the effect of immunomodulatory therapy in 40 women with autoimmune POI in Scandinavia.
We hope that positive results from this study will lead to rituximab becoming a standard treatment for women with POI.
Women with Neurological Disease and Medication Safety during Pregnancy
Contact person: Marte-Helene Bjørk
Epilepsy and Migraines Affect Up to One in Four Women of Childbearing Age
Uncertainty about the safety of medications for these conditions during pregnancy means that many women do not receive effective treatment.
Previous research has shown that some anti-seizure medications, such as valproate (marketed as Orfiril in Norway), which is effective for epilepsy and migraines, carry a high risk of birth defects such as spina bifida and neurodevelopmental disorders like autism. This has led to restrictions on its use for women across Europe unless no alternatives are available. It is essential to identify which newer and effective anti-seizure medications can be used safely by women.
Professor Marte-Helene Bjørk, a neurologist, led the SCAN AED project, which compiled extensive health registry data on all children born in the Nordic countries. Bjørk and her team examined which medications the mothers of these five million children used and what diagnoses the children later received.
Their research found that certain anti-seizure medications appear to be safe, such as:
- Lamotrigine (Lamictal)
- Levetiracetam (Keppra)
These are safe when used alone or in combination.
However, children exposed to topiramate (Topamax) during pregnancy had a significantly increased risk of both birth defects and conditions like autism and intellectual disabilities. These findings led to the introduction of a new pregnancy prevention program for topiramate in Europe in early 2023. Topiramate is used to treat migraines and epilepsy.
Impact on Clinical Guidelines
Major changes to international clinical treatment guidelines for these conditions are anticipated, ensuring safer treatment options for women.
The SCAN AED project was funded by NordForsk.
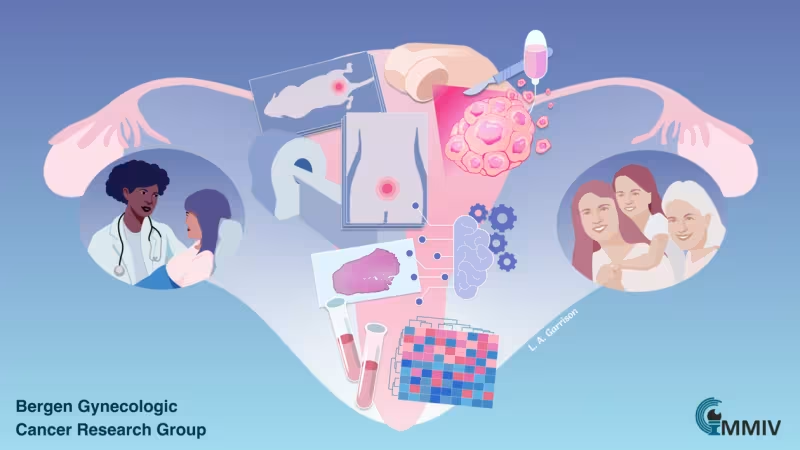
Bergen Research Group for Gynecological Cancer
The research group is led by Professor Camilla Krakstad at the Department of Clinical Science and the Centre for Cancer Biomarkers (CCBIO), University of Bergen (UiB). The group also has strong ties to the Women's Clinic at Haukeland University Hospital in Bergen.
The team focuses on gynecological cancer, with a particular emphasis on improving diagnosis and treatment for patients with uterine cancer.
The research is built on three key pillars:
- Expert Researchers: A diverse and passionate team dedicated to making discoveries that benefit patients.
- Clinical Collaboration: Strong partnerships with clinical departments enable the collection of samples and data from relevant patients.
- Engaged Patients: Positive patient participation, with individuals willingly contributing to research efforts.
The research community includes both clinicians and basic scientists, who collaborate using various methods to generate new knowledge about gynecological cancers.
Recent Achievements
- Biomarkers: The team has identified several promising biomarkers to improve diagnosis and tailor treatments more effectively.
- Clinical Studies: Contributions to clinical trials and investigations of how treatments affect patients' quality of life in the years following a cancer diagnosis.
- Imaging: Close collaboration with Professor Ingfrid S. Haldorsen's team at the Mohn Imaging and Visualization Center to explore the use of radiological data for better diagnostics.
Areas of Focus
Mechanisms of Cancer Spread and Treatment Resistance:
- Use of advanced cell models and genetic analyses to study changes associated with aggressive diseas
Improving Treatment Outcomes:
- Research aimed at optimizing therapeutic strategies and identifying patients who would benefit most from specific interventions.
The research group includes approximately 25 members and receives funding from:
- University of Bergen (UiB)
- Western Norway Regional Health Authority (Helse Vest)
- The Norwegian Cancer Society (Kreftforeningen)
- The Research Council of Norway (Norges forskningsråd)
- The Trond Mohn Research Foundation
The group is dedicated to advancing knowledge in gynecological cancer for the ultimate benefit of patients.
Vulvar Cancer
Contact person: Daniela Elena Costea
Cancer of the External Female Genital Organs (Vulva and Vagina): A Rare and Under-Researched Cancer
Cancers originating in the external female genital organs (vulva and vagina) are rare, with limited research dedicated to them. However, the incidence of this cancer type is steadily increasing, particularly among women under 60. In Norway, approximately 80 patients are diagnosed with these cancers annually.
Despite the heterogeneity of this disease, most patients receive the same standard treatment. Unfortunately, the prognosis remains poor due to the lack of effective treatments for locally advanced, radiation-resistant diseases or systemic disease. One of the major challenges is understanding why patients with similar disease characteristics experience differing outcomes despite undergoing the same primary treatment regimen.
Biomarkers for stratifying patients have not yet been identified for this cancer type. The research group is focused on:
- Defining biomarkers for personalized treatment.
- Establishing representative experimental models to better understand the biology of this cancer and to test new drugs.
The Role of Organoids
Organoids are three-dimensional in vitro tissue culture models that closely mimic the original tumors. They offer a promising tool for selecting personalized treatments.
One of the group’s main objectives is to establish an organoid platform for vulvar cancer, which will:
- Serve as the foundation for identifying the biological properties of these tumors.
- Help characterize potential responses to specific medications.
- The team aims to use organoids to identify treatments tailored to individual patients.
- This cutting-edge approach combines experimental pathology and clinical insights to improve outcomes for women with vulvar cancer.
This work is a collaboration between the Experimental Pathology Research Group, led by Daniela Elena Costea at the Gade Laboratory for Pathology, University of Bergen (UiB), and Professor Line Bjørge at the Women’s Clinic, Haukeland University Hospital, and the Department of Clinical Medicine 2, UiB.
For further insights, read Printer mini-svulster i 3D for å finne medisin mot vulvakreft | Norske Kvinners Sanitetsforening (sanitetskvinnene.no) (external link) (In Norwegian).

